$22 M of Potential Fraud, Waste and Abuse Discovered in 2012 Medicare Ophthalmology Claims
In 2012, approximately 49 million Medicare claims were related to screening, diagnosis or treatment of cataracts, wet acute macular degeneration and/or glaucoma. Medicare paid approximately $3.5 billion for these particular services.
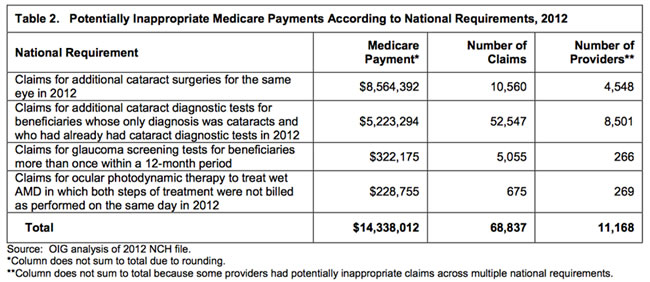
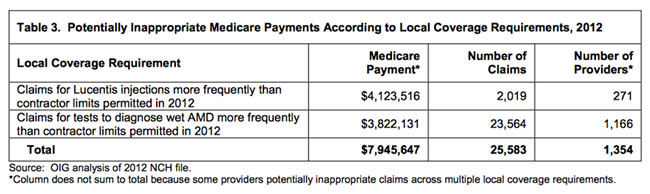
Review of the data using 4 National Coverage Requirements found $14 million in potentially inappropriate payments and according to 2 Local Coverage Requirements an additional $8 million dollars were detected in erroneous payments. Although these requirements were put in place to prevent such fraud, waste and abuse, the Medicare contractors paid these claims that clearly did not fit the criteria.
The 4 National Coverage Requirements:
The 2 Local Coverage Requirements:
Specifically, two of eleven contractors paid a significant proportion of these improper claims. Each of these highest paying contractors had most of the potentially improper claims related to one of the Local Coverage Requirements.
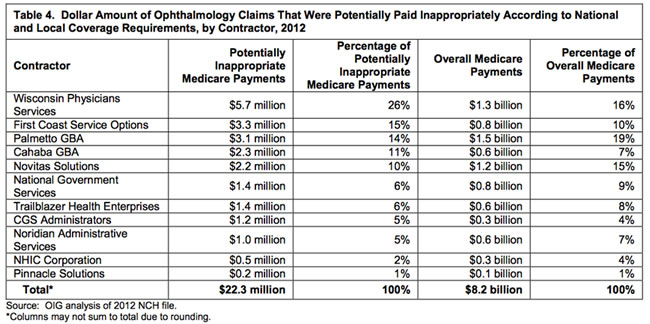
Below lists the Medicare payments by the individual Medicare contractors.
Although the contractors cannot manually review each individual claim, prevention of improper payments should include medical review actions of selected claims and provider outreach and education by the Medicare contractors. OIG ‘s recommendations to CMS as a result of this review are as follows:
- Implement additional claims processing edits or improve existing edits to ensure claims are paid appropriately (based on NCDs and LCDs)
- Prevent payment for cataract surgery on beneficiary who has already had natural lens removed
- Prevent payment for Ocular photodynamic therapy claims in which both steps not performed on same day
- Prevent payments for additional cataract diagnostic tests for those whose only diagnosis was cataracts and already had cataract tests in the calendar year
- Prevent payment for glaucoma screening for beneficiaries more than once in 12-month period
- Determine the appropriateness of ophthalmology claims identified in this OIG report and take appropriate action
- Recoup an inappropriate payment
- Provider education on billing for ophthalmology services
- No action if determined to be appropriate payment with necessary documentation to explain medical need
CMS agrees with these recommendations as part of its continued commitment to prevent fraud, waste and abuse. The Medicare contractors will continue with One Program Integrity (One PI) and the Fraud Prevention System (FPS) to review Medicare data with analytic tools and to use predictive analytic technology to identify billing behaviors that may be suspicious.