CMS Just Announced New Provider Enrollment Provisions
As of December 3, 2014, new safeguards have been added to the CMS provider enrollment policies. CMS continues to focus on prevention of Medicare fraud, waste and abuse as part of their comprehensive program integrity plan. Reportedly, 25,000 providers have already been excluded from participation and may no longer be able to re-enroll.
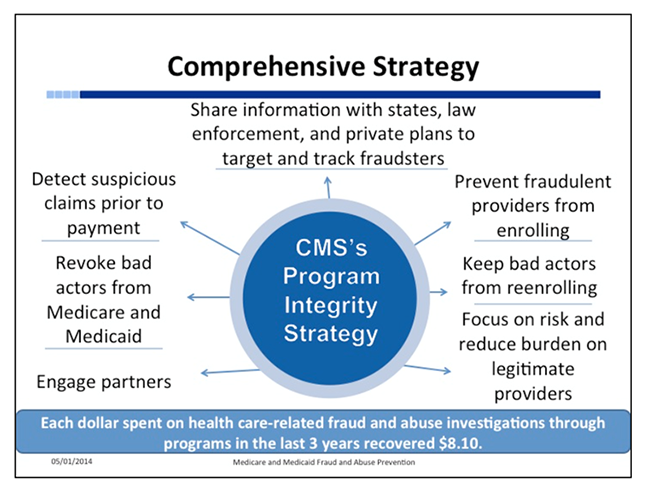
Use of the Fraud Prevention System, a predictive analytics technology has been able to identify any potential fraudsters and revoke enrollment prior to any money being paid. An additional preventive measure includes determining specific geographic areas that show an unusually high rate of fraud designating these as Medicare fraud hot spots. In these hot spots, CMS has stopped new enrollments of ambulance suppliers (Houston and Philadelphia) and home health providers (Fort Lauderdale/Miami, Detroit, Dallas, Houston and Chicago) to allow time for a thorough investigation of existing entities and providers including fingerprint–based technology for background checks.
The new changes according to CMS are as follows:
- Adding the ability to deny the enrollment of providers, suppliers, and owners affiliated with an entity that has unpaid Medicare debt. This will help prevent individuals and entities from being able to incur substantial debt to Medicare, leave the Medicare program and then re-enroll as a new business to avoid repayment of the outstanding Medicare debt. CMS will only enroll otherwise eligible individuals or entities if they repay the debt or enter into a repayment plan.
- Adding the ability to deny the enrollment or revoke the billing privileges of a provider or supplier if a managing employee has been convicted of certain felony offenses. This provision ensures that CMS can block or remove bad actors from the Medicare program to protect beneficiaries and safeguard the Medicare Trust Funds.
- Permitting CMS to revoke billing privileges of providers and suppliers that have a pattern or practice of billing for services that do not meet Medicare requirements. This is intended to address providers and suppliers that regularly submit improper claims in such a way that it poses a risk to the Medicare program.
- Making the effective date of billing privileges consistent across certain provider and supplier types. Most practitioners and practitioner groups may only submit bills as of the filing date of their enrollment application or the date of first furnishing services at a new practice location, whichever is later. CMS is now eliminating ambulance suppliers’ previous ability to bill for up to a year prior to enrollment in the Medicare program. Also, CMS now requires that ambulance providers and other provider and supplier types submit any claims within 60 days of the revocation of their billing privileges, consistent with the requirements for practitioners and practitioner groups. This provision is estimated to save $327 million annually.
Exclusion from the federal healthcare programs can be avoided if your compliance program is ongoing and effective, identifying any areas of potential fraud, waste or abuse, instituting corrective action to mitigate risks and initiating the self-disclosure protocol, likely reducing fines and penalties.
