Infographic: MACRA- Understanding the MIPS Impact
On October 14, 2016, the Department of Health and Human Services (HHS) issued its final rule implementing the MACRA Quality Payment Program. Most providers following the traditional Medicare payment model will now be using the Merit-based Incentive Payment System (MIPS). CMS estimates approximately 500,000 clinicians will be eligible to participate in MIPS in the first year of the program.
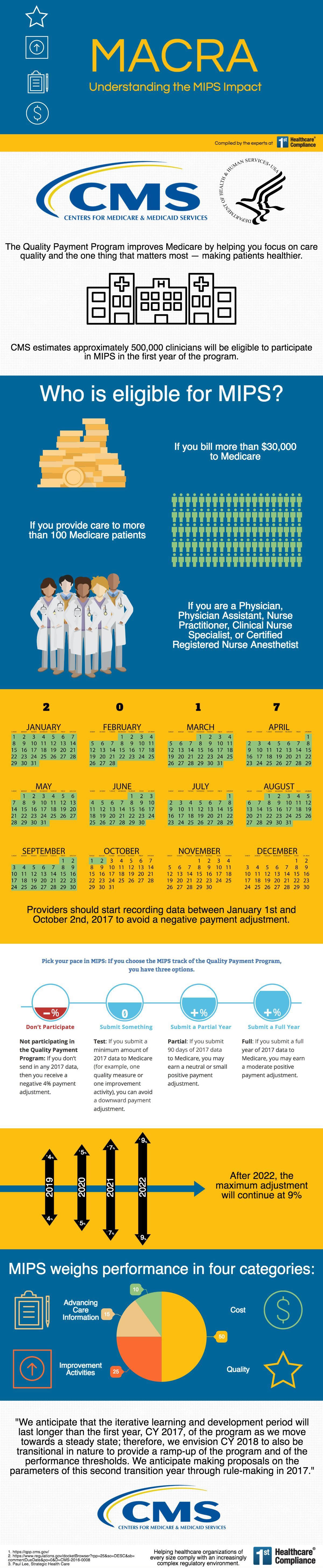
Providers will be eligible for MIPS if: they bill more than $30,000 to Medicare annually, they provide care to more than 100 Medicare patients, and they are a physician, physician assistant, nurse practitioner, clinical nurse specialist, or certified registered nurse anesthetist. Reporting under MIPS should start in 2017. In order to avoid a negative payment adjustment, providers need to start recording data between January 1st and October 2nd, 2017. Payment adjustments will be based on the amount of data that is submitted during the reporting year. Maximum adjustment levels will start at a lower percentage and increase annually until the new maximum of +/- 9% is reached in 2022. MIPS weighs performance based on four categories: Quality (50%), Improvement Activities (25%), Advancing Care Information (15%), and Cost (10%).