Improper Payments for Evaluation & Management Services Cost Medicare Billions in 2010
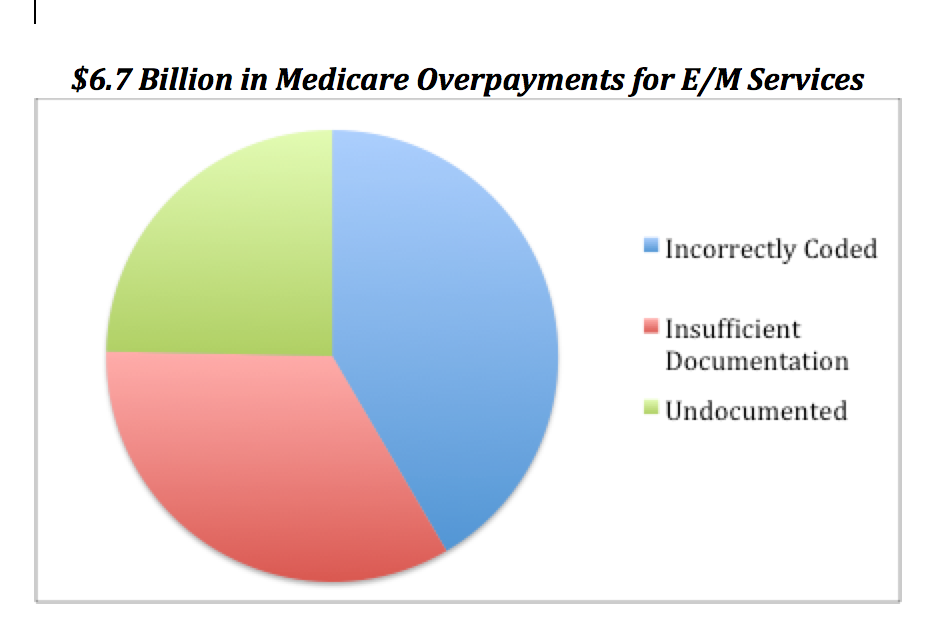
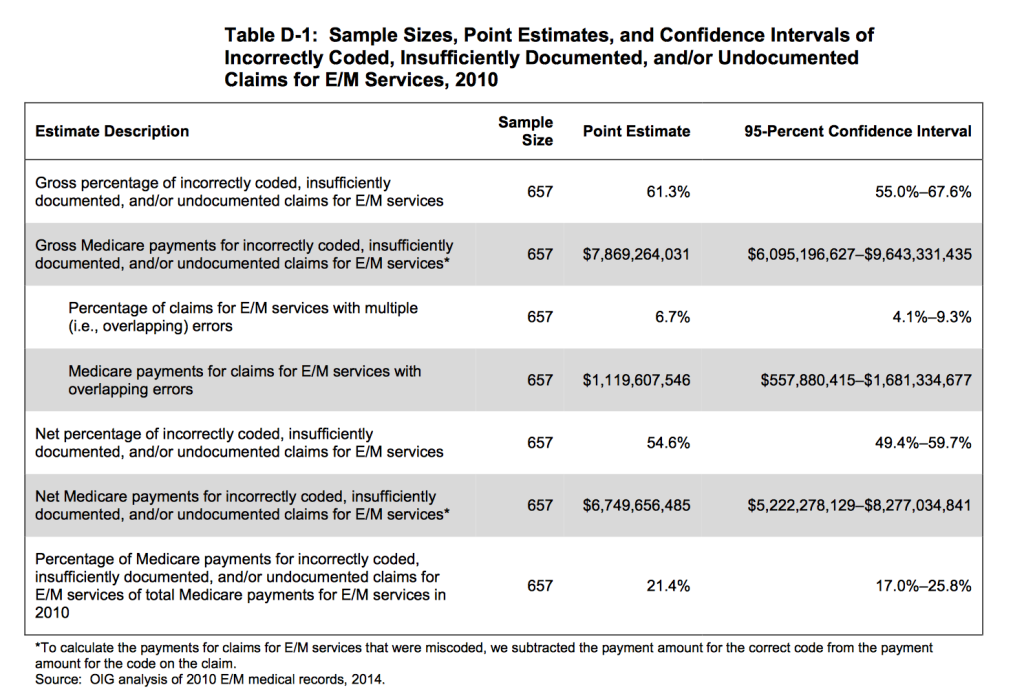
According to the Office of the Inspector General’s report for 2010, Evaluation and Management services accounted for 30% of Medicare Part B payments, a total cost of $32.3 billion. However, 55% of these 370 million claims were coded incorrectly and/or lacked appropriate documentation. These claims correlated to $6.7 billion in improper Medicare payments.
26% of total 2010 Medicare claims were upcoded and 15% downcoded. Inadequate documentation to support medical necessity and appropriateness was identified in 12% and no documentation discovered in 7%. Incorrect coding and unbundling was found in 2%.
The groups were divided into “high-coding physicians” (those coding 95% of claims as Level 4 or 5) and “other physicians”. High-coding physicians’ claims were much more likely to contain errors, almost always related to upcoding. Insufficent documentation was also found to be more likely in high-coding physicians. Compared to the last 10 years, all physicians coded at higher levels in all types of visits.
The documentation must support the level of service, medical necessity and appropriateness. Physicians can use either the 1995 or 1997 Documentation Guidelines. Any services rendered since September 2013 can use a combination with extended history of present illness from the 1997 Guidelines and other criteria from 1995 Guidelines. A handwritten or electronic signature or signature attestation is required for sufficient documentation.
E/M services should be medically reasonable and necessary and appropriate coding must meet the specific CPT requirements.
The level depends on :
- extent of patient history
- extent of physical exam
- complexity of medical decision-making
- counseling
- coordination of care
- nature of presenting problem
- time