Webinar Q&A: Credentialing and Provider Enrollment
First Healthcare Compliance hosted an interactive webinar “I & A, NPPES, PECOS and CAQH, Oh My!: Credentialing and Provider Enrollment Necessities” with Josh Plummer, President and CEO, and Michelle Pivelja, CPCS, the Director of Credentialing for PracticeWorx. Click here to view the webinar.
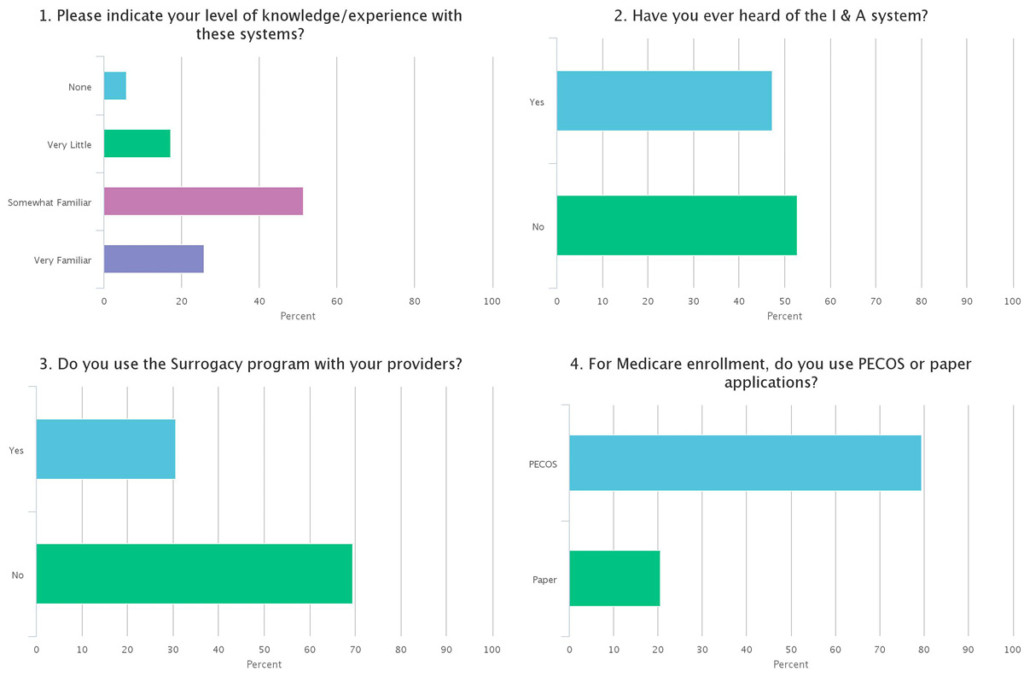
Here are polling results of the attendees when asked about I&A, NPPES, PECOS and CAQH:
The experts at PracticeWorx, Josh and Michelle, provide answers to commonly asked questions regarding credentialing and provider enrollment.
How long does it take to enroll a provider?
This question is always asked by our clients. And the only definitive answer we can give them is that it varies. There are many variables such as the particular insurer, whether this is a new grad or an experienced provider, is the provider joining an existing group or is this a new practice, or even the time of year you’re trying to enroll. However, we do have some average enrollment timeframes based upon our experiences. For a new grad enrolling with Medicare for the first time, we anticipate 90-120 days upon submitting a clean and complete application through PECOS. An existing provider re-assigning benefits to a new group averages about 75 days (we have seen this accomplished with certain MACs in 45 days). Commercial insurers have the widest ranges of course. We have experienced some insurers that only take 30 days to add a provider to an existing group, but if it’s a new provider with a new group it could take 150-180 days. Overall, we advise our clients that the average enrollment time is 100 days from submission of clean, complete applications.
Do I enroll as a group or an individual?
This is a common question with providers starting up a new practice. Our advice in this situation is that if there is any chance in the future of adding an associate or partner to the practice, then go ahead and spend the time now to set up a group (organization) and enroll the group as well as the individual provider.
If I have a CAQH profile, do I still have to enroll separately with insurers?
The simple answer is yes. Some insurers don’t use CAQH. And for those insurers that do, most still have a requirement to complete the insurer’s specific credentialing application. However, utilizing CAQH usually allows the credentialing application to be less extensive, and it will also make the re-credentialing process quite a bit easier with those insurers who utilize CAQH.