Are You Familiar With the New CMS Payment Model?
The new CMS payment model ties reimbursement to value instead of volume. The focus is on developing a payment method based on quality and improvement of the delivery of care. The increasing ability to share information amongst providers, consumers and others, necessitates the dual function of “best possible” decision making and maintaining patient privacy.
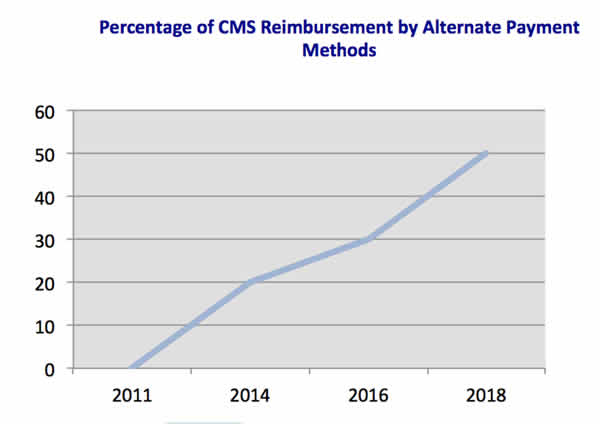
HHS states a goal of 30 % of all fee- for- service Medicare payments to go through alternative payment methods such as bundled payments or ACOs by the end of 2016 and 50 % by the end of 2018. Even higher goals are set for hospital payments based on Hospital Value Based Purchasing and the Hospital Readmission Reduction Program. The target for hospitals is 85% by the end of 2016 and 90% by 2018.
The new Health Care Payment Learning and Action Network has been formed to get input from providers, consumers, private payers, employers, and state Medicaid programs to create fair alternative payment methods. This move toward a patient centered approach should improve care coordination and communication. According to Debra Ness, President of the National Partnership for Women and Families, “it will give patients and families the information, tools and supports they need to make better decisions, use their healthcare dollars wisely and improve health outcomes.” (Source: HHS press release Jan 26, 2015)
An obvious goal is to avoid waste related to duplicative or unnecessary tests or screenings, but the ability for patients to choose their provider or location of their service based on quality metrics is even more significant. The Quality Entity (QE) program allows organizations with this designation to access Medicare data to publish comparative performance reports on the providers or hospitals. This means consumers can now access cost and charge data for physician services and hospitals.
Cost savings from these alternative payment methods are demonstrated through data. Preliminary estimates show a decrease of healthcare spending in ACO programs that have been single-handedly attributed to $417 million in savings. With regard to all of the quality initiatives instituted from 2010 to 2013, HHS reports an overall $12 billion in savings. Additional benefits include 1.3 million fewer patient harms, decreased hospital readmissions and 50,000 lives saved.